What is polycystic ovary syndrome?
Polycystic ovary syndrome (PCOS) is a severe genetic, hormone, metabolic and reproductive disorder that affects women and girls.
PCOS can affect a woman’s ability to produce eggs. In addition, it is linked with higher levels of circulating insulin, characteristic of type 2 diabetes.
The precise etiology of PCOS is unknown. The key is to have an early diagnosis.
Obtaining treatment once diagnosed along with weight loss may lower the risk of long-term complications such as type 2 diabetes and heart disease.
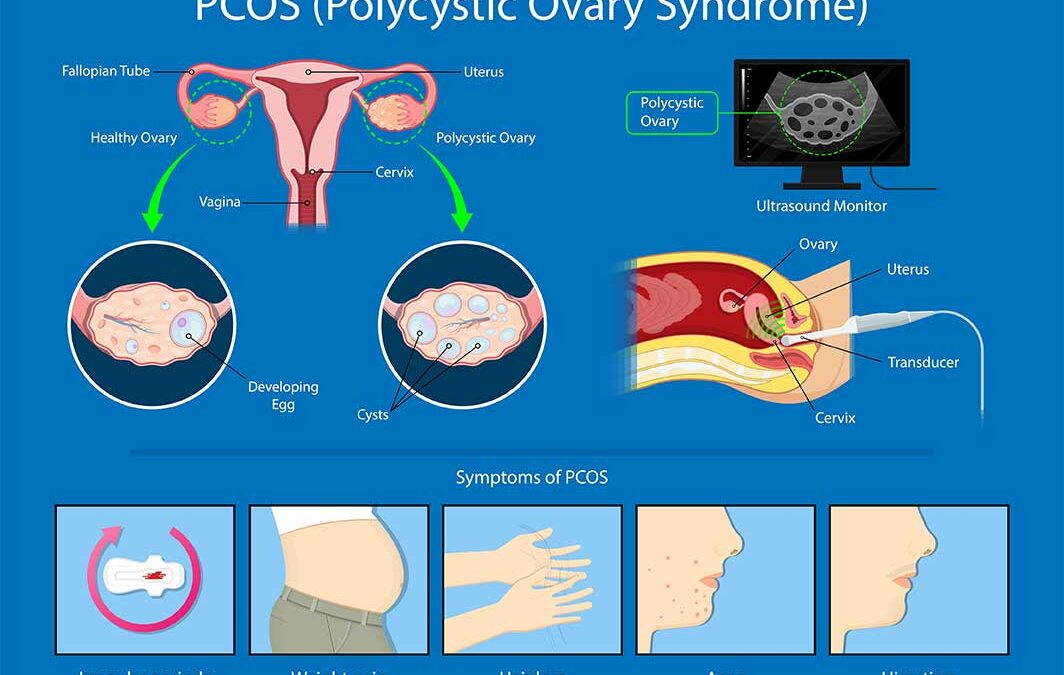
This condition affects women’s ovaries, causing an abnormal number of cysts on the ovaries’ surface.
The cysts are follicles that contain undeveloped eggs on your ovaries.
Polycystic Ovarian Disease often results in a sporadic release of eggs from the ovaries.
However, in some women, PCOS may prevent any eggs from being released.
PCOS is a treatable condition, and a healthy lifestyle is vital in the treatment.
What are the symptoms of PCOS?
PCOS symptoms of PCOS may include one or more of the following:
- Irregular or loss of periods
- Fertility problems
- Weight gain
- Hirsutism (excessive hair growth)
- Thinning of or loss of hair
- Acne
When should I see a doctor?
It is recommended to make an appointment with a health care provider if you’re worried about your periods, lack of ability to become pregnant, or if you have high androgen levels (hyperandrogenism).
Symptoms might include new hair growth on your face and body, acne, and male-pattern baldness.
How is PCOS Diagnosed?
The appearance of two or more of the following three conditions can lead to a diagnosis of PCOS:
- Many cysts develop around the edge of the ovaries (polycystic ovaries)
- Failure in ovulation (release of eggs)
- A higher level of male hormones or more than normal active male hormones
A diagnosis of PCOS will typically involve several tests, including blood tests, blood pressure checks, and ultrasound sound scans.
The recommendation is that all women with PCOS receive a screening to assess their risk of type 2 diabetes.
Yearly screening is recommended for:
- Family history of type 2 diabetes
- Obesity
- Gestational Diabetes diagnoses
What causes PCOS?
Weight gain and insulin resistance are two contributing factors to PCOS. Typically insulin resistance causes the body to produce more insulin than usual (hyperinsulinemia).
Higher insulin levels can cause ovaries to produce too much testosterone, impairing regular ovulation. Although generally, testosterone is regarded as a male hormone, all women have testosterone, albeit in lower quantities than men.
Increased insulin levels can also cause weight gain, typically associated with developing type 2 diabetes and PCOS.
One sign of insulin resistance is dark, velvety patches of skin on the lower part of the neck, armpits, groin, or under the breasts. An enormous appetite and weight gain may be other signs.
What is the treatment for PCOS?
Treatments for PCOS can vary. Lifestyle changes will be recommended, particularly in overweight patients. Shedding some pounds helps reduce insulin levels and improve symptoms.
A low carbohydrate lifestyle is effective for lowering insulin levels. In addition, this change helps with weight loss and is likely to have additional benefits on other symptoms of PCOS.
Exercise is a dual benefit for people with type 2 diabetes—walking, running, taking the stairs, and parking further away in the parking lot.
This physical activity can push glucose out of your blood and into your cells. The CDC recommends getting at least 150 mins a week of brisk walking or similar exercise, which comes out to about 30 mins a day, five times a week.
Medication may also be prescribed to help with different symptoms.
Specific contractive pills or anti-androgen drugs may be advised if hormones are not correctly balanced.
Fertility problems can also be treated by the following means:
- Clomifene is a fertility medication that can help to induce ovulation.
- Laparoscopic ovarian drilling (LOD) is a surgical procedure that can restore ovulation.
- In vitro fertilization (IVF) may be required if the above is not successful or not appropriate.
The Center for Diabetes and Endocrine Care is here for all your endocrine and diabetic needs or questions. We have provided a link for you to make an appointment online or feel free to give one of our team members a call: 954-963-7100

Recent Comments